Irradiated Corneal Tissue: Benefits for Your Patients and Your Practice
Abstract
A challenge to corneal transplantation is the availability of safe and suitable donor tissue. While about 133,000 corneas are recovered from donors per year, problems with short shelf life, poor tissue quality, and possible contamination result in only 69% of these being transplanted.1 Tissue irradiation, such as that used in Lions World Vision Institute’s (LWVI’s) OptiGraft® line of irradiated sterile tissue, has proven to be the most effective means of ensuring the integrity and quality of tissue, extending its shelf life, and reducing the risk of infection and tissue rejection.
The demand for corneal transplants is huge. So why is donated tissue being discarded?
Corneal diseases impact over 6 million people, yet only 1 out of every 70 corneal transplants needed worldwide are fulfilled.2,3 According to The 2018 Eye Banking Statistical Report, over 85,000 corneal transplants were performed in the United States alone in the year 2018.1 However, out of 133,000 recovered corneas, only 69% were transplanted.1 This low transplant rate is due to several factors, including short shelf life, low quantity and quality of donor tissues, and increased risk of donor contaminated tissue.4
Tissue banks have responded to these issues by implementing corneal sterilization techniques such as pressured vapor sterilization, gas plasma sterilization, and radiation.5 Out of these options, tissue irradiation has largely been the most successful sterilization technique. Tissue irradiation has been used for over five decades as a verified, standard method of sterilization for medical products.6,7 Several studies have found that irradiation does not negatively affect the quality or integrity of tissue.4,8-12 Furthermore, these studies suggest the use of sterile irradiated corneas would increase the amount of transplantable corneal tissue, decrease donor immunogenicity and risk of infection, and increase long-term tissue storage.4,9
Irradiation Sterilization Increases Tissue Availability and Usability
Too often, donor corneal tissue can’t be transplanted due to poor tissue quality, specifically low endothelial cell count, thereby decreasing the already low supply of transplantable tissue.9,14 Irradiation sterilization allows such tissue to be used for nonendothelial purposes such as patch grafts or lamellar grafts.9,10,13,14 Irradiation targets the cells’ DNA bonds, thus killing epithelial and endothelial cells while preserving the integrity of the tissue. Utine et al. reported pull-through testing of irradiated corneas used for lamellar keratoplasty was as strong as fresh (Optisol-stored) corneas.13 In another study, Chae et al. compared the biological and physical characteristics of gamma-irradiated corneas to fresh corneas and concluded that the elastic modulus, hydration, and light transmittance were of similar quality between fresh and irradiated corneas.4 Sikder et al. found comparable stromal histology, pachymetry, and ultrastructural characteristics in irradiated corneas and fresh corneas.11 Calhoun et al. discovered that light transmission and attenuation were very similar in fresh and irradiated corneas.8 Furthermore, in a short-term study of irradiated sterile corneas, Daoud et al. found that the macroscopic quality and clarity of the transplanted tissues were not affected by tissue irradiation.9 And while Tran et. al found a slight increase in light scattering in e-beam irradiated corneas, this increase was ultimately deemed insignificant to the quality of the tissue.10 Hence, sterilization by irradiation essentially increases the available supply of quality, transplantable-ready tissues for patch and lamellar surgeries.
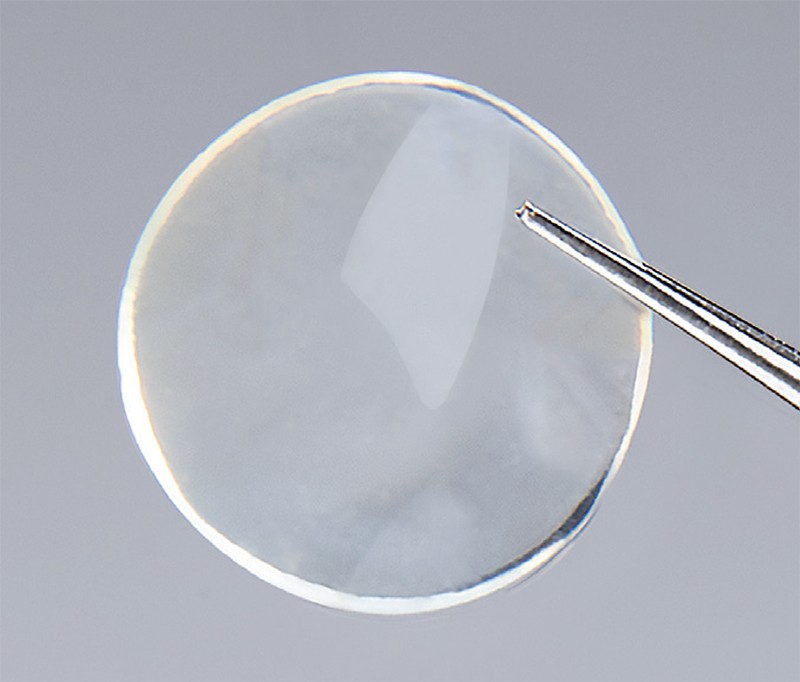
Sterile clear corneal allograft
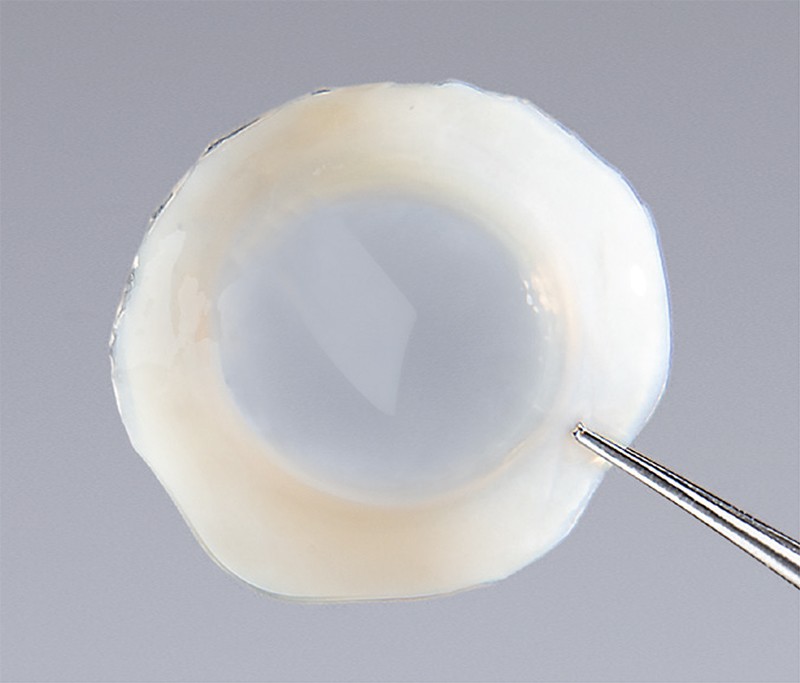
OptiGraft whole moon full thickness with a scleral rim provides sterile option for lamellar keratoplasty and KPro procedures.
Irradiated Tissue Prevents Immune Rejection
Another consideration for surgeons performing fresh tissue corneal transplants is the imminent risk of graft failure due to recipient immune rejection.4 The immunosuppressive effect of irradiation sterilization directly addresses this concern.12 Irradiation sterilization decreases donor immunogenicity by killing the antigen-presenting cells and keratocytes that trigger immune responses in transplant recipients.4,9 When antigen-presenting cells are depleted, direct sensitization is avoided, consequently decreasing the possibility of graft rejection.13 Stevenson et al. found that T-cells isolated from irradiated allografts exhibited no secondary alloimmune response.12 The reduced risk of immune rejection characteristic of sterile corneas is especially beneficial for patients who have had multiple transplantations or may already be immunocompromised.
Irradiated Tissue Reduces Infection Risk
Currently, the standard method of fresh cornea storage is in Optisol. Corneal grafts may also be preserved in glycerin. Neither preservation method, however, eliminates the risk of infection.10 Irradiation sterilization may reduce the risk of transplant infections by eliminating the microbes found in the donor tissue.10 This is especially relevant to the eye bank industry now because of the strict regulations for the procurement, storage and handling of donor tissues currently being implemented to reduce risk of infection.10 It’s possible that some of these regulations could be revised to reflect the decreased risk of transmission from using sterile corneas.
Irradiated Tissue Offers Reliable Clinical Outcomes
In a 7- to 36-month follow-up study of lamellar keratoplasty using sterile irradiated corneas, not only did all grafts remain clear and re-epithelialize, but no immune or graft rejections were noted.13 Clinical outcomes for corneal patch grafts resulted in epithelialization within a few days with no evidence of de-epithelialization, infection, or rejection.9 E-beam irradiated corneas used as patch grafts in glaucoma drainage device (GDD) surgery were found to have comparable clinical outcomes to more commonly used scleral patches.15 No increase in patch graft erosion was found when irradiated corneas were used in place of scleras.15 Two prominent studies have been performed on the clinical outcomes of sterile cornea use in Boston type 1 keratoprosthesis (KPro). The first, Akpek et al. found sterile corneas to be a viable alternative for fresh corneas used in KPro procedures.16 This study had an average follow-up of 16.5 months, during which time no patients experienced graft failure. In the second study, Fadlallah et al found several positive clinical outcomes for KPro cases using sterile corneas: Over a post-operative period of 1 year, visual acuity improved in 94% of the cases, there was an overall retention percentage of 94.1%; and no incidence of infection or necrosis occurred in any of the cases.7 Most recently, Mathews et al. studied the long-term clinical outcomes of irradiated corneas in 9 patients who underwent DALK, ALK, and KPro surgeries.14 The study noted the successful use of sterile corneas for various etiologies including infectious keratitis, non-inflammatory corneal conditions, and inflammatory or autoimmune keratitis.14 Interestingly, the study also suggested the possible use of sterile corneas to temporize the eye when infectious keratitis or sterile keratolysis are present until either complete eradication or total immunosuppression is attained.14 Lastly, irradiated corneas hold promise for therapeutic penetrating keratoplasty use.14
Ready to Use With a Long Shelf Life, Irradiated Tissue is a Practical Solution
Fresh, Optisol-stored corneas must be transplanted within 14 days of preservation, which restricts opportunities for their use.9 Moreover, the tissue must be preserved in solution and refrigerated in temperatures between 2 – 8°C. These requirements pose challenges for tissue transport and storage. Another option for tissue storage is glycerin, which can last much longer. However, glycerin-preserved corneas have a noticeably rubbery feel and may be difficult to handle during surgery.9 Even more problematically, they must be allowed to rehydrate prior to transplantation and are not sterile.13
Tissue irradiation eliminates these problems. It has been found to extend the shelf life of the tissue for up to 2 years without affecting its texture or readiness for use.4 Because irradiated tissues are stored in human albumin, they do not require rehydration and can be stored at room temperature, making them ready for anytime use.4 These characteristics are particularly beneficial for surgery centers with limited refrigerated storage and remote communities that can benefit from storing these tissues in large quantities. Additionally, studies have found no noticeable difference between the visualization of text through irradiated, long-term stored corneas (20 months) and through fresh corneas.10 The tolerance of irradiated corneas to long-term storage make them ideal for emergency, trauma, and tumor resection cases. Moreover, in a mission trip to Lebanon, Fadlallah et al. found visual acuity improvement in 94.1% of cases when using irradiated corneas as carriers for the Boston type 1 keratoprosthesis, with no incidence of stromal necrosis or infectious keratitis.7
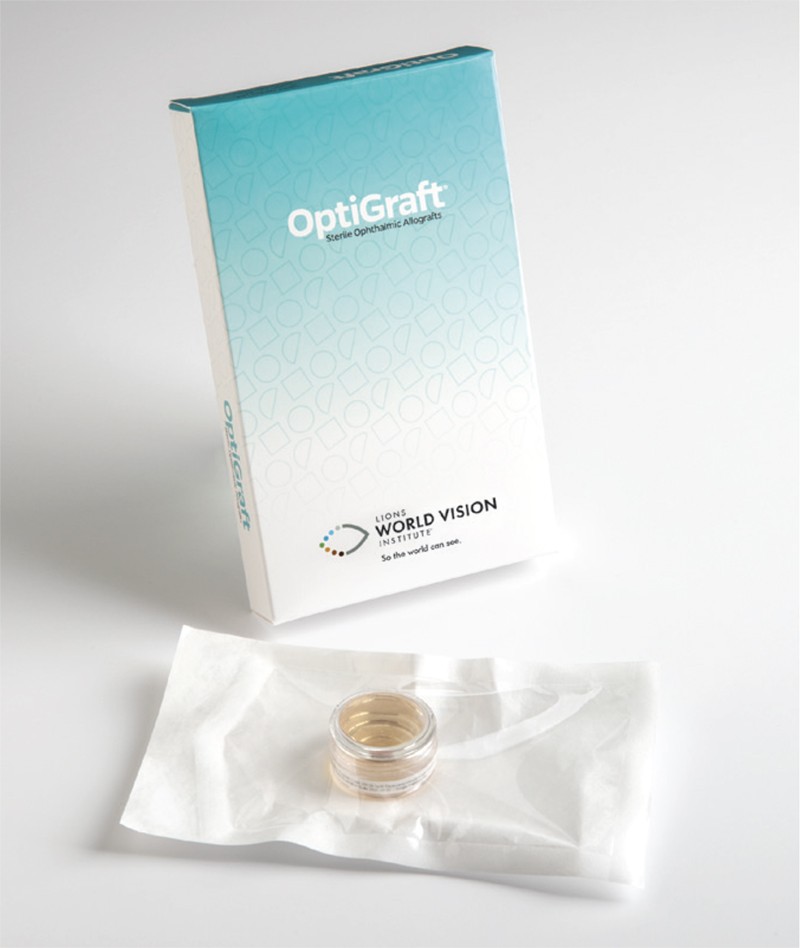
OptiGraft sterile corneal tissue has an extended shelf life for up to two years and can be stored at room temperature.
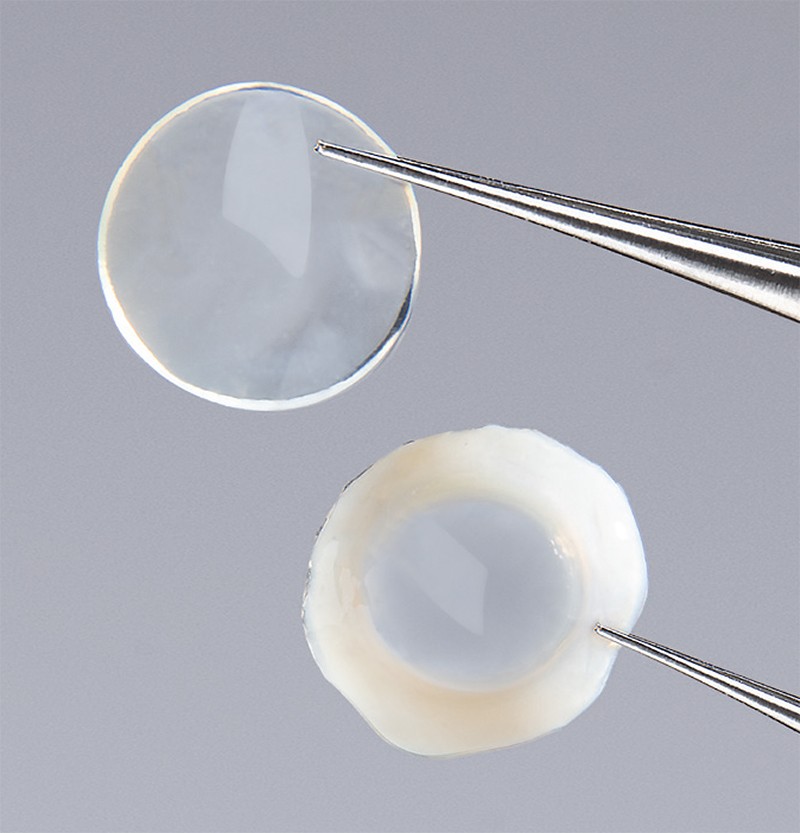
OptiGraft sterile clear corneal tissue: whole moon split thickness (top) and whole moon full thickness with a scleral rim (bottom)
E-Beam vs. Gamma Radiation: What You Should Know
While many studies have focused on evaluating the effects of gamma irradiation on corneal donor tissues, electron beam (e-beam) irradiation has risen in popularity in the past several years, particularly for use with corneal patches in glaucoma drainage device (GDD) procedures.15,17 Both methods are valid sterilization techniques. However, the biggest difference between them is the tissue exposure time. Gamma-irradiated tissues are subject to greater exposure times than e-beam-treated tissue because gamma irradiation dose rates are much lower than those used for e-beam irradiation, thus requiring longer exposure times.18 E-beam irradiation exposes the tissues to high dose rates of irradiation at a low penetration for much shorter exposure times, making the e-beam process more effective and efficient. A minor disadvantage posed by the longer exposure periods of gamma-irradiated tissues, however, is the formation of minor changes in corneal collagen matrix.10 E-beam irradiation has not been found to result in noticeable differences in the collagen matrix of corneas, thereby leaving important clinical properties such as clarity and light scattering unaffected.12 In fact, when surgeons examined long-term stored corneas for intact stroma, opacities, and overall structural integrity prior to surgery, they found no difference between sterile and fresh corneas.10
OptiGraft: The Clear Choice
Sterile irradiated corneas, such as those in LWVI’s new OptiGraft line, provide a more flexible approach to corneal transplants by permitting a longer shelf life and decreased immunogenicity at a much lower cost than fresh corneal tissues and other sterile tissues available. Their longer shelf life and ambient storage capability allows immediate access, making them a practical option for remote communities and mission trips, as well as for emergency and trauma surgeries.7 Unlike glycerin-preserved and Optisol-stored corneas, irradiated corneas do not require re-hydration or special handling techniques for transplantation. And in addition to these benefits, OptiGraft products also offer ease of use through specially designed packaging. Additionally, the ability of irradiation sterilization to remove antigens can potentially increase the corneal tissue supply by allowing a wider range of tissues to be made suitable for transplantation. Ideally, all tissue donated should be used for transplant, honoring and maximizing the donor’s gift.
References
- 2018 Eye Banking Statistical Report. Eye Bank Association of America. https:// restoresight.org/what-we-do/publications/statistical-report/. Published 2019. Accessed February 18, 2020.
- Porth JM, Deiotte E, Dunn M, Bashshur R. A Review of the Literature on the Global Epidemiology of Corneal Blindness. Cornea. 2019;38(12):1602–1609. doi:10.1097/ ICO.0000000000002122
- Gain P, Jullienne R, He Z, et al. Global Survey of Corneal Transplantation and Eye Banking. JAMA Ophthalmol. 2016;134(2):167–173. doi:10.1001/jamaophthalmol.2015.4776
- Chae JJ, Choi JS, Lee JD, et al. Physical and Biological Characterization of the Gamma-Irradiated Human Cornea. Cornea. 2015;34(10):1287–1294. doi:10.1097/ ICO.0000000000000555
- Silindir M, Özer A Y. Sterilization methods and the comparison of e-beam sterilization with gamma radiation sterilization. Fabad J Pharm Sci. 2009; 34(1):43-53
- Singh R, Singh D, Singh A. Radiation sterilization of tissue allografts: A review. World J Radiol. 2016;8(4):355–369. doi:10.4329/wjr.v8.i4.355
- Fadlallah A, Atallah M, Cherfan G, Awwad ST, Syed ZA, Melki SA. Gamma-irradiated corneas as carriers for the Boston type 1 keratoprosthesis: advantages and outcomes in a surgical mission setting. Cornea. 2014;33(3):235–239. doi:10.1097/ICO.0000000000000065
- Calhoun WR, Akpek EK, Weiblinger R, Ilev IK. Evaluation of broadband spectral transmission characteristics of fresh and gamma-irradiated corneal tissues. Cornea. 2015;34(2):228–234. doi:10.1097/ICO.0000000000000323
- Daoud YJ, Smith R, Smith T, Akpek EK, Ward DE, Stark WJ. The intraoperative impression and postoperative outcomes of gamma-irradiated corneas in corneal and glaucoma patch surgery. Cornea. 2011;30(12):1387–1391. doi:10.1097/ICO.0b013e31821c9c09
- Tran KD, Li Y, Holiman JD, et al. Light scattering measurements in electron-beam sterilized corneas stored in recombinant human serum albumin. Cell Tissue Bank. 2018;19(1):19–25. doi:10.1007/s10561-017-9666-x
- Sikder S, McCally RL, Engler C, Ward D, Jun AS. Evaluation of Irradiated Corneas Using Scatterometry and Light and Electron Microscopy. Cornea. 2011;30(5):503–507. doi:10.1097/ICO.0b013e3181eadd0f
- Stevenson W, Cheng SF, Emami-Naeini P, et al. Gamma-irradiation reduces the allogenicity of donor corneas. Invest Ophthalmol Vis Sci. 2012;53(11):7151–7158. Published 2012 Oct 1. doi:10.1167/iovs.12-9609
- Utine CA, Tzu JH, Akpek EK. Lamellar keratoplasty using gamma-irradiated corneal lenticules. Am J Ophthalmol. 2011;151(1):170–174.e1. doi:10.1016/j.ajo.2010.08.007
- Mathews PM, Fogla R, Samayoa E, VanCourt S, Akpek EK. Long-term clinical outcomes of keratoplasty using gamma-irradiated corneal lenticules. BMJ Open Ophthalmol. 2019;4(1):e000396. Published 2019 Nov 10. doi:10.1136/bmjophth-2019-000396
- Passo RM, Hoskins ZB, Tran KD, et al. Electron Beam Irradiated Corneal Versus Gamma- Irradiated Scleral Patch Graft Erosion Rates in Glaucoma Drainage Device Surgery. Ophthalmol Ther. 2019;8(3):421–426. doi:10.1007/s40123-019-0190-x
- Akpek EK, Aldave AJ, Aquavella JV. The use of precut, γ-irradiated corneal lenticules in Boston type 1 keratoprosthesis implantation. Am J Ophthalmol. 2012;154(3):495–498.e1. doi:10.1016/j.ajo.2012.03.022
- Pan Q, Jampel HD, Ramulu P, et al. Clinical outcomes of gamma-irradiated sterile cornea in aqueous drainage device surgery: a multicenter retrospective study. Eye (Lond). 2017;31(3):430–436. doi:10.1038/eye.2016.230
- Odland TL.
Originally published by Lions World Vision Institute
1410 N 21st Street, Tampa, FL 33605-5313, (813) 289-1200


